| MRI B-TFE快速扫描技术和超声检查在正常孕中晚期胎儿侧脑室测量中的应用 |
②. 福建医科大学附属第二医院超声医学科,福建 泉州 362000
侧脑室扩张是产前最常见的脑发育异常,其预后取决于扩张程度[1-3]。目前许多有关胎儿超声方面的研究涉及侧脑室的测量[4]。但孕妇肥胖、有子宫肌瘤、羊水过少、多胎及复杂畸形时,超声对胎儿侧脑室显示较差。胎儿MRI图像因其独特的优势已被证明是产前诊断的重要手段,并被广泛用于产前诊断中[5]。目前,国内外有不少关于MRI(冠状面)测量胎儿侧脑室的报道,但对其横断面测量的报道非常有限。因此,本研究探讨胎儿颅脑MRI(横断面)快速扫描技术与超声(横断面)在胎儿正常侧脑室直径测量中的一致性,论证MRI(横断面)测量胎儿侧脑室的可行性。
1 资料与方法 1.1 一般资料收集2017年1月至2018年10月在我院行MRI检查的胎儿256例,胎龄25~40周,平均34周;孕妇年龄24~38岁,平均29岁。256例胎儿均行MRI(横断面/冠状面)快速扫描及超声检查;超声评估均未见中枢神经系统异常。检查均经孕妇及家属知情同意。
1.2 仪器与方法 1.2.1 MRI扫描使用1.5 T Philips MRI B-TFE快速扫描技术进行扫描。扫描序列和参数:二维快速稳态进动序列和单次快速自旋回波序列,TR 3.5~5.0 ms,TE 1.5~1.8 ms,翻转角5°~60°,带宽125.00 Hz/像素,矩阵236×236或256×256,采集次数2次,层厚4~6 mm,间隔1 mm,FOV 36 cm×36 cm。胎儿头颅横断位及冠状位扫描须在出现完整胎儿形态的基础上再依据胎儿的矢状位重新定位扫描,须在上一个序列扫描完成的基础上进行,在侧脑室水平(脉络丛视野良好)测量[6](图 1,2)。
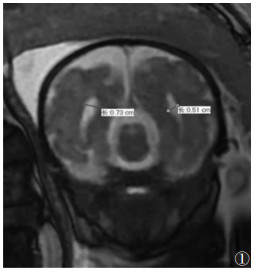 |
| 图 1 胎儿头颅MRI扫描的冠状面,测量侧脑室的直径 |
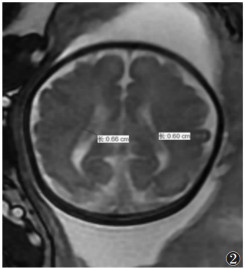 |
| 图 2 胎儿头颅MRI扫描的横断面,测量侧脑室的直径 |
1.2.2 超声检查
使用Philips EPIQ5彩色多普勒超声,在丘脑水平的横断位图像上及脉络丛后缘水平垂直于侧脑室的直线上测量侧脑室。仅测量位于最深半球的侧脑室[7](图 3)。
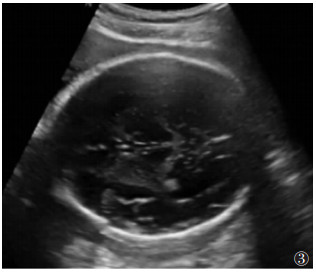 |
| 图 3 胎儿头颅超声成像的轴面,测量侧脑室的直径 |
1.3 图像分析
由3名影像诊断医师分别于超声、MRI图像上测量侧脑室直径,MRI图像测量时取最大一侧的侧脑室直径[8]。测量结果取3名医师测量的平均值。
1.4 统计学分析使用SPSS 13.0统计软件。采用回归分析法分析MRI冠状面所测侧脑室直径与胎龄的关系。采用配对t检验分析MRI横断面与冠状面测量侧脑室直径的差异。利用组内相关系数(Intraclass correlation coefficient,ICC)和Bland-Altman图评价超声(横断面)和MRI图像(冠状面和横断面)在胎儿侧脑室测量上的一致性。以P<0.05为差异有统计学意义。
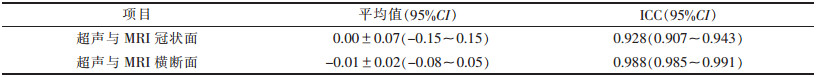
2 结果MRI冠状面与横断面侧脑室直径分别为(0.818±0.149)、(0.801±0.148)mm,冠状面侧脑室直径略大于横断面,差异有统计学意义(t=-3.780,P=0.000)。孕中晚期胎儿的胎龄与MRI冠状面测量的侧脑室直径无相关性(r=0.156)。超声测量侧脑室直径为(0.814±0.141)mm。超声(横断面)与MRI(冠状面和横断面)测量结果的一致性较好(表 1),在Bland- Altman图中无特别趋势(图 4,5)。
| 表 1 MRI(冠状面、横断面)和超声测量(横断面)侧脑室直径的一致性分析 |
 |
 |
| 图 4 超声横断面与MRI冠状面侧脑室直径测量的Bland-Altman图(横坐标:超声横断面与MRI冠状面测量值之和除以2;纵坐标:超声横断面与MRI冠状面测量值之差) |
 |
| 图 5 超声横断面与MRI横断面侧脑室直径测量的Bland-Altman图(横坐标:超声横断面与MRI横断面测量值之和除以2;纵坐标:超声横断面与MRI横断面测量值之差) |
3 讨论
侧脑室的形态受大脑生长的影响,因此侧脑室测量有助于评估胎儿大脑的生长和区域分化,是产前诊断的关键。研究[9-13]表明,在妊娠中晚期,胎儿侧脑室直径相对固定,不受胎龄的影响,因此,在此期间侧脑室直径的测量相对准确。本研究孕中晚期胎儿的胎龄与MRI冠状面测量的侧脑室直径无相关性,与文献[14-16]报道一致。
超声是产前诊断的主要方法,但检查结果易受操作者水平等的影响。MRI软组织分辨力高、无电离辐射、扫描视野大,且不受操作者水平的影响,已越来越多地应用于胎儿产前诊断中[14-16]。但由于孕妇不能使用镇静剂和对比剂,不适合憋气及各种门控,如呼吸门控和心电门控,且长时间扫描易产生运动伪影。MRI B-TFE快速扫描序列在一次90°射频脉冲后即可完成K空间的填充,一般在几秒内即出现图像,即使孕妇不憋气也无明显运动伪影,图像清晰。在胎儿MRI头颅标准化扫描中,通常先扫描任意一个体位的胎头,以此为基础,结合母体的三平面位置,扫描胎儿头部3个体位。本研究所需胎儿头颅横断面及冠状面图像即在胎儿矢状面上定位进行扫描,进而得出两侧对称的图像。
Weisstanner等[17]在2016年提出胎儿侧脑室的MRI测量可模拟超声的测量方法,选择侧脑室扩张的胎儿作为研究对象,结果表明,超声横断面测量胎儿侧脑室与MRI横断位测量结果基本一致;MRI横断面可作为测量侧脑室扩大的一种方法。以上研究并未选择无脑室扩张的胎儿,因此,本研究选取256例无脑室扩张的胎儿进行MRI检查,分别在横断面和冠状面图像上测量其侧脑室。结果表明,超声(横断面)和MRI(冠状面、横断面)侧脑室测量的重复性好,结果相似,ICC值分别为0.928、0.988,与文献[8, 12-13]报道一致。配对t检验显示,MRI横断面与冠状面测量结果差异有统计学意义(P<0.05),即MRI横断位同样能准确测量胎儿侧脑室直径,进一步验证了Weis- stanner等[17]的观点。
综上所述,MRI B-TFE快速扫描序列在胎儿侧脑室测量中与超声检查结果一致性较好,且能够弥补超声检查的不足,可在短时间内得到质量较好的胎儿MRI图像,已成为胎儿产前诊断的重要方法。
| [1] |
Beeghly M, Ware J, Soul J, et al. Neurodevelopmental outcome of fetultrasoundes referred for ventriculomegaly[J]. Ultrasound Obstet Gynecol, 2010, 35: 405-416. |
| [2] |
Melchiorre K, Bhide A, Gika AD, et al. Counseling in isolated mild fetal ventriculomegaly[J]. Ultrasound Obstet Gynecol, 2009, 34: 212-224. |
| [3] |
Perlman S, Shashar D, Hoffmann C, et al. Prenatal diagnosis of fetal ventriculomegaly:agreement between fetal brain ultrasonography and MR imaging[J]. AJNR Am J Neuroradiol, 2014, 35: 1214-1218. |
| [4] |
Guibaud L. Fetal cerebral ventricular measurement and ventriculomegaly:time for procedure standardization[J]. Ultrasound Obstet Gynecol, 2009, 34: 127-130. |
| [5] |
朱铭. 磁共振技术在产前诊断中应用新进展[J]. 实用妇产科杂志, 2018, 34(11): 811-813. |
| [6] |
Gaglioti P, Oberto M, Todros T. The significance of fetal ventriculomegaly:etiology, short- and long-term outcomes[J]. Prenat Diagn, 2009, 29: 381-388. |
| [7] |
Weichert J, Hartge D, Krapp M, et al. Prevalence, characteristics and perinatal outcome of fetal ventriculomegaly in 29, 000 pregnancies followed at a single institution[J]. Fetal Diagn Ther, 2010, 27: 142-148. |
| [8] |
Perlman S, Shashar D, Hoffmann C, et al. Prenatal diagnosis of fetal ventriculomegaly:agreement between fetal brain ultrasonography and MR imaging[J]. AJNR Am J Neuroradiol, 2014, 35: 1214-1218. |
| [9] |
Taketani K, Yamada S, Uwabe C, et al. Morphological features and length measurements of fetal lateral ventricles at 16-25 weeks of gestation by magnetic resonance imaging[J]. Congenit Anom Kyoto, 2015, 55: 99-102. |
| [10] |
赵芳, 王将军. 磁共振成像在产前胎儿颅脑疾病的临床应用价值[J]. 实用医学影像杂志, 2019, 20(1): 15-17. |
| [11] |
Behrendt N, Zaretsky MV, West NA, et al. Ultrasound versus MRI:is there a difference in measurements of the fetal lateral ventricles?[J]. J Matern Fetal Neonatal Med, 2017, 30: 298-301. |
| [12] |
Tilea B, Alberti C, Adamsbaum C, et al. Cerebral biometry in fetal magnetic resonance imaging:new reference data[J]. Ultra-sound Obstet Gynecol, 2011, 37: 173-181. |
| [13] |
Yaniv G, Katorza E, Bercovitz R, et al. Region-specific changes in brain diffusivity in fetal isolated mild ventriculomegaly[J]. Eur Radiol, 2016, 26: 840-848. |
| [14] |
Atallah A, Lacalm A, Massoud M, et al. Prenatal diagnosis of pericallosal curvilinear lipoma:specific imaging pattern and diagnostic pitfalls[J]. Ultrasound Obstet Gynecol, 2018, 51: 269-273. |
| [15] |
Shekdar K, Feygin T. Fetal neuroimaging[J]. Neuroimaging Clin N Am, 2011, 21: 677-703. |
| [16] |
van Doorn M, Oude Rengerink K, Newsum EA, et al. Added value of fetal MRI in fetuses with suspected brain abnormalities on neurosonography:a systematic review and meta-analysis[J]. J Matern Fetal Neonat Med, 2016, 29: 2949-2961. |
| [17] |
Weisstanner C, Kasprian G, Gruber GM, et al. MRI of the fetal brain[J]. Clin Neuroradiol, 2015, 25: 189-196. |
 2020, Vol. 18
2020, Vol. 18


