| 脑淋巴瘤病临床特点及MRI表现的系统评价 |
原发性中枢神经系统淋巴瘤(primary central nervous system lymphomas,PCNSL)是少见的仅限于中枢神经系统的结外非霍奇金淋巴瘤,占所有原发性脑肿瘤的2%~3%[1]。普遍认为典型的PCNSL为幕上单发或多发结节/肿块,边界清,水肿较轻,增强扫描呈显著均匀强化[2]。但实际工作中会出现不典型PCNSL,造成诊断困难。脑淋巴瘤是PCNSL的一种少见亚型[3],1999年Bakshi等[4]首次提出脑淋巴瘤这一概念。此后,陆续出现脑淋巴瘤病的个案或小样本病例报道[5-44],但对该病的系统描述较少。本研究汇总分析Pubmed数据库中有关脑淋巴瘤的文献,结合我院3例,采用系统评价的方法综合分析其临床及影像学特点,以提高对该病的认识。
1 资料与方法 1.1 文献检索 1.1.1 资料来源计算机检索Pubmed数据库,搜集1989年1月至2019年7月发表的有关脑淋巴瘤的英文文献。以“lymphomatosis cerebri”、“primary cen- tral nervous system lymphomas”、“brain lymphoma”等为检索词进行检索。
1.1.2 文献筛选标准入选标准:①全文文献,至少有首次MRI平扫T2WI/T2 FLAIR及增强扫描图像;②MRI表现为病变范围较广,至少累及3个脑叶或3个解剖区域;③增强扫描无强化或见少许补丁样强化,无结节或肿块样强化灶;④组织病理学确诊为淋巴瘤。排除标准:①全身系统性淋巴瘤患者;②血管内淋巴瘤患者。
1.2 资料提取由2名经验丰富的影像诊断医师独立筛选文献、提取资料,如遇分歧,经讨论作出决定。资料提取内容主要包括临床资料、影像表现及病理结果。影像学分析内容包括病灶位置、分布、形态学、MRI信号、强化特点及随访图像等。
2 结果共42篇(50例)符合入选标准;加上我院3例,共53例纳入分析。53例中,男26例,女27例,男女比例0.96:1;年龄19~85岁,平均(48.0±20.4)岁;其中4例有免疫缺陷病史。临床主要首发症状为认知下降(27例,50.9%)、步态不稳(20例,37.7%)、头痛(6例,11.3%)、癫痫发作(3例,5.7%)。19例同时有2种及以上主要症状。
患者从首发症状至第1次行MRI检查的平均时间约52 d。首次MRI检查除4例(7.5%)主要表现为幕下异常,余49例(92.5%)均有双侧大脑半球浸润,其中25例(47.2%)同时有幕上、幕下浸润,表现为至少3个脑叶或3个解剖区域的脑白质弥漫性T2WI/T2 FLAIR高信号,主要涉及大脑半球深部和侧脑室周围白质(图 1a),侵及皮质下白质24例(45.3%)、胼胝体21例(39.6%)、基底节区24例(45.3%)、丘脑15例(28.3%)、脑干23例(43.4%)、小脑13例(24.5%)、脊髓6例(11.3%)。17例有平扫T1WI图像,其中7例以等信号为主,10例以低信号为主。首次MRI增强扫描,病变区无强化32例(60.4%)(图 1b),呈轻微线样或补丁样强化21例(39.6%)。
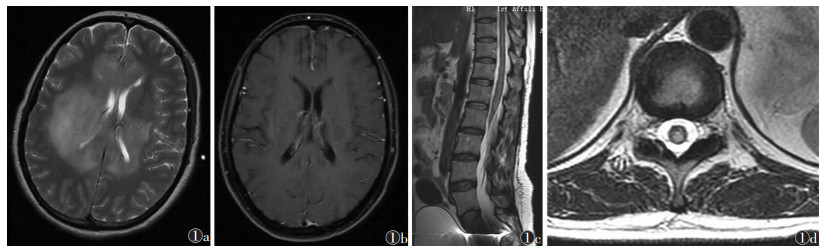 |
| 图 1 女,38岁,活检确诊为弥漫大B细胞淋巴瘤 图 1a 首次MRI检查,横轴面T2WI示大脑半球白质区弥漫稍高信号 图 1b 首次MRI增强扫描未见明显异常强化 图 1c,1d 分别为首次MRI检查后2个月后腰椎MRI T2WI矢状位及横轴位图像,示腰段脊髓呈异常高信号 |
33例有随访MRI图像,未确诊脑淋巴瘤前,26例MRI显示进展,5例显示病变范围缩小,2例无明显变化。显示进展26例中,16例病变沿皮质脊髓束向下延伸至基底神经节、丘脑、中脑、脑桥、延髓和小脑半球,甚至进入脊髓(图 1c,1d);7例病变通过胼胝体延伸浸润。33例中21例首次MRI增强扫描无强化,其中16例随访时MRI增强扫描异常强化,5例呈明显斑片状强化,11例呈结节或肿块样强化;12例首次MRI增强扫描略有补丁样或线样强化病灶,随访MRI增强扫描呈明显斑片状强化3例,多发结节强化9例。
53例脑淋巴瘤中,37例(包括我院3例)经脑活检病理确诊,15例经尸检确诊,1例未描述病理采样方法。其中6例第1次活检尚无定论,经第2次活检或尸检后确诊;1例活检2次无结论,在尸检时确诊。43例(81.1%)为B细胞淋巴瘤,9例(17.0%)为T细胞淋巴瘤,1例(1.9%)未进一步分类。患者从出现首发症状至活检的平均时间为3.9个月,从发病至确诊约4.5个月。37例镜下病理图片示肿瘤细胞弥漫分布在白质中,高倍镜下可见有突出细胞核的单个分散的圆形肿瘤细胞,既不聚合也不形成肿块,无坏死。可见3种肿瘤细胞浸润模式:①18例呈弥漫性分散浸润;②15例呈血管周围分布,肿瘤细胞呈袖套样排列,向邻近脑实质浸润;③4例呈弥漫密集分布。
28例(52.8%)在诊断为脑淋巴瘤前曾行类固醇激素治疗,部分症状及影像学表现一度好转,后加重。脑活检确诊的37例中,11例(29.7%)接受放射治疗,26例(70.3%)接受化疗。患者平均生存时间<24个月,我院1例生存时间为4年。
3 讨论脑淋巴瘤是PCNSL的少见亚型,其人口统计学特征与PCNSL相似,男女比例相当。以往文献[6]报道该病的平均发病年龄约57岁,而本系统评价为(48.0±20.4)岁,可能与近几年发表文献中的患者及我院患者年龄较轻有关。本组仅4例有免疫缺陷病史[7],说明脑淋巴瘤发生可能与个体的免疫状态无关。
脑淋巴瘤最常见的临床表现是进行性认知功能下降和步态异常,而常见于其他原发性脑肿瘤的临床表现,如持续性头痛、癫痫发作、恶心或呕吐等,在脑淋巴瘤中较少出现,可能与其肿瘤细胞弥漫浸润较少形成肿块、一般不会引起明显占位效应及颅高压有关。
脑淋巴瘤的MRI常表现为浸润双侧大脑半球深部及脑室周围白质区的T2WI/T2 FLAIR弥漫性高信号,病变分布似乎具有在整个中枢神经系统弥漫性浸润侵袭的倾向,还可见皮质下白质、U型纤维、胼胝体侵犯[8-10],甚至灰质也可受累。因此,有学者[11]认为脑淋巴瘤应命名为弥漫性PCNSL。其病变常沿皮质脊髓束扩展,在随访患者的MRI报告中,描述了病变扩展沿皮质脊髓束延伸至基底神经节、丘脑、中脑、脑桥、延髓和小脑半球,甚至进入脊髓[12-13]。Chen等[14]报道的患者同时表现出沿皮质脊髓束向上和向下扩散的趋势。
首次MRI增强扫描,脑淋巴瘤常无强化或呈少许补丁样、线样强化[6, 15-16],一般无具体肿块样强化灶。通常认为对比增强模式主要依赖于血-脑脊液屏障渗透率、中枢神经系统病变的血管范围及肿瘤细胞结构,其中血-脑脊液屏障渗透率是主要因素。镜下所见肿瘤细胞浸润的3种模式(弥漫性分散浸润、血管周围分布和弥漫密集分布),可解释该病的强化模式[11]。当肿瘤细胞弥漫性浸润未导致血-脑脊液屏障显著破坏时,MRI无明显强化[5, 14, 17-19]。而FLAIR高信号病变区域呈点状和曲线样强化可能表明由内皮细胞的直接损伤引起的小血管血管屏障破坏[20]。随访MRI逐渐呈明显斑片状强化甚至单个或多个结节状、肿块样强化[13, 21-22],这是该病进展的表现。而LI等[11]提到5例确诊的PCNSL,早期表现为单发或多发肿块样强化伴弥漫白质脑病,随访MRI表现为弥漫浸润性病变,推测这些不同的强化模式可能发生在疾病发展的各个阶段,且首次MRI增强扫描上的不强化或非肿块样强化可能仅是弥漫性浸润性PCNSL的特殊模式。
目前,诊断脑淋巴瘤的金标准仍是脑组织病理学检查,然而,由于这种组织学形式较少见,及时准确诊断仍较困难。脑淋巴瘤多为B细胞淋巴瘤,镜下淋巴细胞浸润脑实质稀疏分布,无肿块形成,表现为局灶性倾向血管周围分布[23]。由于有更多的反应性小淋巴细胞和巨噬细胞,脑淋巴瘤在组织学上需与血管炎及病毒性脑炎鉴别。另外,血管周围袖套征并非总存在于脑淋巴瘤中,病毒性脑炎也可有此表现[24]。因此,只有免疫组化评估提示了恶性淋巴细胞,才能作出正确诊断。
与其他原发恶性肿瘤相比,脑淋巴瘤的诊断常有较长的延迟时间,约4.5个月,原因可能为:①脑淋巴瘤的临床表现易用痴呆或抑郁解释,通常不立即行神经影像学检查。②即使行MRI检查,根据其MRI表现也易被误诊为其他疾病,如传染性或炎性疾病、自身免疫性脑病[15, 21, 24-25]、中毒或代谢紊乱[18]、血管病变[23, 26-27]、神经退行性疾病[28]、胶质瘤病等,常需进一步检查或动态观察确认诊断。③若初始诊断为炎性脱髓鞘等疾病,使用糖皮质激素冲击治疗,细胞毒性作用使得包括淋巴瘤细胞等细胞大量凋亡,可能造成活检时延误诊断[6]。
脑淋巴瘤预后较差,大多数患者死于诊断后的6个月内[15]。早期诊断和使用大剂量的甲氨蝶呤适当治疗是影响预后的最重要因素。Izquierdo等[6]研究表明,年龄较小(<56岁)者、更高的卡氏功能状态评分、甲氨蝶呤治疗和B细胞组织学是较好结局的独立预后因素;早期诊断为LC的患者接受大剂量甲氨蝶呤治疗后较未使用者总生存期更长,分别为13.80个月(0.70~56个月)和2.95个月(0.33~56个月)。
总之,脑淋巴瘤是一种PCNSL亚型,临床工作中常被误诊或延误诊断,应提高对其临床及影像表现的认识,如遇有进行性认知功能障碍患者,MRI示双侧半球非对称性弥漫白质异常,有沿皮质脊髓束浸润整个中枢神经系统倾向,增强扫描无强化或轻度非肿块样强化,且无全身和传染性疾病证据时,应想到脑淋巴瘤的可能。早期脑活检可将脑淋巴瘤的诊断延迟时间最小化,及早接受大剂量甲氨蝶呤治疗可延长患者生存期。
| [1] |
Bathla G, Hegde A. Lymphomatous involvement of the central nervous lymphomatous involvement of the central nervousl system[J]. Clin Radiol, 2016, 71: 602-609. |
| [2] |
Haldorsen IS, Krakenes J, Krossnes BK, et al. CT and MR imaging features of primary central nervous system lymphoma in Norway, 1989-2003[J]. Am J Neuroradiol, 2009, 30: 744-751. |
| [3] |
Neelakantan S, Kumaran SP, Viswamitra S, et al. Myriad of MR imaging phenotypes of primary central nervous system lymphoma in a cohort of immunocompetent Indian patient population[J]. Indian J Radiol Imaging, 2018, 28: 296-304. |
| [4] |
Bakshi R, Mazziotta JC, Mischel PS, et al. Lymphomatosis cerebri presenting as a rapidly progressive dementia:clinical, neuroimaging and pathologic findings[J]. Dement Geriatr Cogn Disord, 1999, 10: 152-157. |
| [5] |
Giglio P, Bakshi R, Block S, et al. Primary central nervous system lymphoma masquerading as herpes encephalitis:clinical, magnetic resonance imaging, and pathologic findings[J]. Am J Med Sci, 2002, 323: 59-61. |
| [6] |
Izquierdo C, Velasco R, Vidal N, et al. Lymphomatosis cerebri:a rare form of primary central nervous system lymphoma. Analysis of 7 cases and systematic review of the literature[J]. Neuro Oncol, 2016, 18: 707-715. |
| [7] |
Kawakami T, Sakai K, Mimura Y, et al. Development of primary central nervous system lymphoma associated with human immunodeficiency virus and JC virus infection[J]. J Clin Exp Hematop, 2014, 54: 211-217. |
| [8] |
Lewerenz J, Ding XQ, Matschke J, et al. Dementia and leukoencephalopathy due to lymphomatosis cerebri[J]. J Neurol Neurosurg Psychiatry, 2007, 78: 777-778. |
| [9] |
Miki Y, Tomiyama M, Kurotaki H, et al. Primary central nervous system lymphoma mimicking Bickerstaff's encephalitis[J]. Neurol Sci, 2014, 35: 139-141. |
| [10] |
Kawai N, Kawanishi M, Tamiya T, et al. Usefulness of[J]. Ann Nucl Med, 2005, 19: 415-419. |
| [11] |
Li L, Rong JH, Feng J. Neuroradiological features of lymphoma tosis cerebri:a systematic review of the English literature with a new case report[J]. Oncol Lett, 2018, 16: 1463-1474. |
| [12] |
Rivero SE, Torralba CM, Sanjuan PF, et al. Lymphomatosis cere bri mimicking iatrogenic Creutzfeldt-Jakob disease[J]. BMJ Case Rep, 2014, 2014: 2013201246. |
| [13] |
Imperiale D, Taraglio S, Atzori C, et al. Diffuse leukoencephalo pathy due to lymphomatosis cerebri:a clinicopathological repo rt[J]. Neurol Sci, 2015, 36: 1071-1073. |
| [14] |
Chen H, Dong H. A rare case of nonenhancing primary central nervous system lymphoma mimic multiple sclerosis[J]. Neuros ciences (Riyadh), 2015, 20: 380-384. |
| [15] |
Murakami T, Yoshida K, Segawa M, et al. A case of lymphoma tosis cerebri mimicking inflammatory diseases[J]. BMC Neurol, 2016, 16: 128. |
| [16] |
Yu H, Gao B, Liu J, et al. Lymphomatosis cerebri:a rare variant of primary central nervous system lymphoma and MR imaging features[J]. Cancer Imaging, 2017, 17: 26. |
| [17] |
Raz E, Tinelli E, Antonelli M, et al. MRI findings in lymphom atosis cerebri:description of a case and revision of the literatu re[J]. J Neuroimaging, 2011, 21: e183-e186. |
| [18] |
Leschziner G, Rudge P, Lucas S, et al. Lymphomatosis cerebri presenting as a rapidly progressive dementia with a high meth ylmalonic acid[J]. J Neurol, 2011, 258: 1489-1493. |
| [19] |
Carlson BA. Rapidly progressive dementia caused by nonenhan cing primary lymphoma of the central nervous system[J]. AJNR Am J Neuroradiol, 1996, 17: 1695-1697. |
| [20] |
Taieb G, Duran-Pena A, de Chamfleur NM, et al. Punctate and curvilinear gadolinium enhancing lesions in the brain:a practic al approach[J]. Neuroradiology, 2016, 58: 221-235. |
| [21] |
Yamamoto T, Kojima K, Koibuchi K, et al. A case of primary central nervous system lymphoma presenting diffuse infiltrative leukoencephalopathy[J]. Intern Med, 2012, 51: 1103-1106. |
| [22] |
Ge J, Zuo C, Guan Y, et al. Enhanced MRI and 18F-FDG PET/CT findings of primary central nervous system lymphoma mimi cking encephalitis[J]. Clin Nucl Med, 2016, 41: e436-e438. |
| [23] |
Rollins KE, Kleinschmidt-Demasters BK, Corboy JR, et al. Lymp homatosis cerebri as a cause of white matter dementia[J]. Hum Pathol, 2005, 36: 282-290. |
| [24] |
Pandit L, Chickabasaviah Y, Raghothaman A, et al. Lymhomato sis cerebri——a rare cause of leukoencephalopathy[J]. J Neurol Sci, 2010, 293: 122-124. |
| [25] |
Imataki O, Uchida S, Yokokura S, et al. Central nervous system peripheral T cell lymphoma manifesting as lymphomatosis cer ebri that was misdiagnosed as Neuro-Behcet's disease:a case report[J]. Case Rep Oncol, 2018, 11: 806-813. |
| [26] |
Lee PJ, Berrios I, Ionete C, et al. Lymphomatosis cerebri:diagn ostic challenges and review of the literature[J]. BMJ Case Rep, 2016, 2016: 2016216591. |
| [27] |
Weaver JD, Vinters HV, Koretz B, et al. Lymphomatosis cerebri presenting as rapidly progressive dementia[J]. Neurologist, 2007, 13: 150-153. |
| [28] |
Kanai R, Shibuya M, Hata T, et al. A case of "lymphomatosis cerebri" diagnosed in an early phase and treated by whole bra in radiation:case report and literature review[J]. J Neurooncol, 2008, 86: 83-88. |
| [29] |
Moulignier A, Galicier L, Mikol J, et al. Primary cerebral lymp homa presenting as diffuse leukoencephalopathy[J]. AIDS, 2003, 17: 1111-1113. |
| [30] |
Vital A, Sibon I. A 64-year-old woman with progressive demen tia and leukoencephalopathy[J]. Brain Pathol, 2007, 17: 117-118, 121. |
| [31] |
Terae S, Ogata A. Nonenhancing primary central nervous system lymphoma[J]. Neuroradiology, 1996, 38: 34-37. |
| [32] |
Sugie M, Ishihara K, Kato H, et al. Primary central nervous sy stem lymphoma initially mimicking lymphomatosis cerebri:an autopsy case report[J]. Neuropathology, 2009, 29: 704-707. |
| [33] |
Clark AJ, Lee K, Broaddus WC, et al. Primary brain T-cell ly mphoma of the lymphoblastic type presenting as altered mental status[J]. Acta Neurochir (Wien), 2010, 152: 163-168. |
| [34] |
Sugino T, Mikami T, Akiyama Y, et al. Primary central nervous system anaplastic large-cell lymphoma mimicking lymphomatosis cerebri[J]. Brain Tumor Pathol, 2013, 30: 61-65. |
| [35] |
Courtois F, Gille M, Haven F, et al. Lymphomatosis cerebri pre senting as a Recurrent Leukoencephalopathy[J]. Case Rep Ne urol, 2012, 4: 181-186. |
| [36] |
Kitai R, Hashimoto N, Yamate K, et al. Lymphomatosis cerebri:clinical characteristics, neuroimaging, and pathological findings[J]. Brain Tumor Pathol, 2012, 29: 47-53. |
| [37] |
Sato H, Takahashi Y, Wada M, et al. Lymphomatosis cerebri with intramedullary spinal cord involvement[J]. Intern Med, 2013, 52: 2561-2565. |
| [38] |
Hai Chen HD. A rare case of nonenhancing primary central ne rvous system lymphoma mimic multiple sclerosis[J]. Neuroscie nces (Riyadh), 2015, 20: 380-384. |
| [39] |
Meng H, Zhou C, Hao Q, et al. A rare case of Primary Central Nervous System Lymphoma initially diagnosed as demyelinating encephalopathy[J]. Neuro Endocrinol Lett, 2015, 36: 124-126. |
| [40] |
Ayuso-Peralta L, Orti-Pareja M, Zurdo-Hernandez M, et al. Cere bral lymphoma presenting as a leukoencephalopathy[J]. J Neu rol Neurosurg Psychiatry, 2001, 71: 243-246. |
| [41] |
Brecher K, Hochberg FH, Louis DN, et al. Case report of unus ual leukoencephalopathy preceding primary CNS lymphoma[J]. J Neurol Neurosurg Psychiatry, 1998, 65: 917-920. |
| [42] |
Kerbauy MN, Pasqualin D, Smid J, et al. Diffuse large B-cell ly mphoma of the central nervous system presenting as "lympho matosis cerebri" and dementia in elderly man:case report and review of the literature[J]. Medicine (Baltimore), 2019, 98: e14367. |
| [43] |
Wanschitz J, Hainfellner JA, Simonitsch I, et al. Non-HTLV-I associated pleomorphic T-cell lymphoma of the brain mimicking post-vaccinal acute inflammatory demyelination[J]. Neuropathol Appl Neurobiol, 1997, 23: 43-49. |
| [44] |
Keswani A, Bigio E, Grimm S. Lymphomatosis cerebri presenti ng with orthostatic hypotension, anorexia, and paraparesis[J]. J Neurooncol, 2012, 109: 581-586. |
 2020, Vol. 18
2020, Vol. 18


